A few months back, I wrote an in-depth piece about histamine intolerances. New research suggests that it may be causing symptoms that seem to be coming from completely different causes including gluten sensitivity.
- Have any questions?
- 480-767-9018
- support@in-goodhealth.com

Are Oxalates To Blame For Inflammation In Your Body?
June 4, 2018
How Much Fuel Do You Need?
July 23, 2018
Are Oxalates To Blame For Inflammation In Your Body?
June 4, 2018
How Much Fuel Do You Need?
July 23, 2018Is Histamine Intolerance Real?
It turns out that histamine from foods can be absorbed. Histamine can cause troubling symptoms that go beyond nocebo (all in your head) reactions1.
Furthermore, histamine intolerance has a history of being underdiagnosed. Some have had it and suffered from symptoms with no concrete explanation for them.
Critical Insight: Many symptoms associated with histamine intolerance are vague. Since there are no tests that can rule it out, it is often overdiagnosed or misdiagnosed.
Histamine Intolerance?
First, I think “histamine intolerance” is an improper phrase. It can be very misleading because it is not a histamine intolerance. It is not an allergy or an autoimmune response to histamine (even if it sounds like it).
Histamine is a normal part of our bodies. To date, no humans have been documented as being intolerant or allergic to histamine. So, this term gives an unclear first impression for those trying to learn.

Bottom Line: The body forms histamine as an essential part of brain cell communication and immune regulation. This normal part of our body is not something that we should fear. Instead, we should be more concerned about its level (rather than its presence).
What Are The Specific Symptoms?

When we think of symptoms involved with this overload of histamine, we primarily look at some of the classic “allergy” symptoms. These include:
- Insomnia
- Dizziness
- Anxiety
- IBS
- Rashes
- Skin flushing
- Palpitations
- Headaches
- Fatigue
- Edema
- Sinus congestion
These are classic symptoms. You could take any one person, give them a mega dose of histamine, and they will start developing them. It is bound to happen, and most importantly of all, they can be life-threatening.
Bottom Line: It is not that people are “intolerant” of histamine. Instead, they simply have too much of it circulating throughout their bodies, where these symptoms take root.
What Are The Vague Symptoms?
Remember when I mentioned that one of the tricks of histamine intolerance is that symptoms are often present? A lot of these vague symptoms can be born from chronic, elevated levels of histamine.
This is where things get murky, but here is what one could expect:
- Changes to the menstrual cycle
- Generalized fatigue
- Headaches and migraines
- Difficulty sleeping
- Having a hard time waking
- Struggling to feel energized
- High blood pressure
- Vertigo and dizziness
- Cardiac palpitations
- Poor regulation of body temperature
- Anxiety, nausea, vomiting, and cramps
Bottom Line: These are all possible symptoms associated with histamine intolerance. It does not mean that they are going to happen – only a possibility. Because they are so general, it is difficult to think of them too precisely.
Why Would Someone Have Too Much?
This idea goes back to the idea that histamine intolerance is less about intolerance and more about having an overload. How would someone end up with more histamine than their body needs?
Think about this: your body has histamine coming in and histamine going out. These are the main two things that your body is in charge of.
Two issues can arise: too much coming in or too little coming out. There would have to be a deficiency on one end, which typically starts with the amount taken.
Let’s pull back some more and start from the beginning. When we think about histamine, we can understand it as a natural response to:
- An allergy
- A chronic infection
- Some sort of chemical trauma to your body
Histamine leaves the body through various enzymes that are in charge of breaking down histamine.
Histamine is a biogenic amine that triggers an inflammatory response in your body to make this happen.
Critical Insight: The problem is that you could easily have too many of these being made and need more being unloaded. The former is more likely, and the latter (due to gene defects) is quite rare.
Understanding DAO Deficiency
A DAO deficiency, which we might understand as a gene defect that makes it difficult for the body to “unload” histamine, may cause histamine overload, triggering all those nasty symptoms previously mentioned.
While they are possible, they are not very probable. Based on my experience with people who think they lack that ability, it is being overly suspected and overdiagnosed.
One of the reasons is that all of those symptoms, the vague ones, could be attributed to many other conditions.
The thing about DAO deficiencies is that they are completely measurable. You can take a test to find out if you have them.
Critical Insight: When it comes to high histamine in the blood, you might see it present, but you cannot always see it – even if it is happening. That is where things get complicated and cause a lot of issues.
What it takes is a lot of judgment, and there is no standard answer that satisfies people across all situations. It is just not that easy.
The thing is that when you consider a diagnosis that you cannot objectively affirm, you have to tread very lightly.
The last thing you want to do is settle on an answer when you are misattributing symptoms that are coming from another cause altogether.
Bottom Line: Something unrelated to histamine intolerance could be causing the same symptoms.
Stress & Anxiety
There are even instances where the other symptoms, like hives and flushing, can come from stress and anxiety.
One can have genuine physical symptoms but misattribute them to a genetic defect (as opposed to something like generalized anxiety).
In the end, these things cut both ways. Many do have these problems that remain undiagnosed, and others fall into the overdiagnosed camp.
Reading yourself into three or four symptoms does not mean you can jump to conclusions, and it always helps to test – suspend judgment until you know the whole story.
How do you diagnose histamine intolerance?

First, you can do it empirically. If you take histamine blockers and feel better, it is not unreasonable to think that histamine intolerance was the root of the problem.
The difficulty here is that histamines have a great deal of influence on your body. It can affect your:
- Overall mood
- State of anxiety
- Stress or panic levels
These are all things that histamines affect and that histamines lower!
This all goes back to the fact that things like anxiety can trigger responses like rashes, and by taking an antihistamine, we can sedate ourselves and feel better (and less anxious).
Even though anxiety was our overall issue, we might attribute it to a histamine intolerance instead.
The other difficulty with histamine is its production in the body. Your body makes histamine in response to allergies, infections, stress, or trauma, but we also get it from some foods.
Certain bacterial events can even make the amine levels in foods lethal, which has caused issues in the past. This thinking, though, has led people to believe that the levels of histamines in certain foods can act as a trigger.

Critical Insight: While it is plausible, many studies have looked at quantifying the level of histamines in foods. These studies, after all their research, are in no way in agreement over what constitutes a “high-histamine food.”
Trends in Foods
Even though we have no data on specific foods, some trends have emerged about foods that are higher in histamines:
- Cured or smoked meats
- Aged cheeses
- Fermented foods
- Shellfish
These are food categories known to be higher in histamines. Does this mean you should avoid them?
If they cause symptoms, they could be relevant. But I really cannot endorse any sort of “histamine food list” because there are just way too many contradictions. The science is just not there yet.
For that reason, I would also not recommend diets that are designed to reduce histamine ingestion just yet.
Because there is so much conjecture about what constitutes a “high-histamine food,” a low-histamine diet would involve cutting out a lot of food- which might not be doing your body any good.
Otherwise, we consider DAO replacement compounds (available as pills) or mast cell stabilizing compounds (high in bioflavonoids).
The cycle is that when mast cells are more stable and less likely to “pop open” with histamine, you are less likely to get symptoms.
Bottom Line: Whether it comes from your diet or other compounds, it is essential to know that histamine intolerance might not be the end of the story. While it might make you feel better, it is just as important to know the root cause of whatever issues you are dealing with – because it might be more than one.
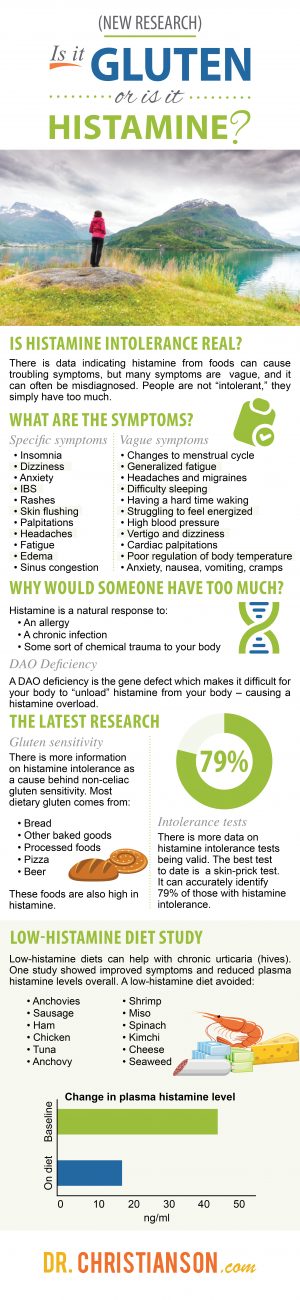
Histamine Intolerance: The Latest Research
While updating this article, I found research that related to two key ideas as it pertains to histamine intolerance. They are:
- There is more information on histamine intolerance as a possible cause of non-celiac gluten sensitivity
- There is more data on histamine intolerance tests being valid (with new tests emerging)
Histamine Intolerance and Gluten Sensitivity
There are many people without celiac disease who have noticed an improvement in digestive symptoms when they follow a gluten-free diet.
While this is good for many reasons, the drawback is that for many people, gluten-free diets end up being lower in fiber and higher in processed fats (on top of being more expensive)2.
Also quite prevalent in these discussions is that gluten-free diets lead to higher risks of diabetes and weight gain. Low-gluten diets may also be associated with a higher risk of type 2 diabetes3.
The truth is that most dietary gluten comes from:
- Bread
- Other baked goods
- Processed foods
- Pizza
- Beer
These same foods are also high in histamine, and they are often seasoned with high-histamine ingredients.
The symptoms of non-celiac gluten sensitivity are similar to those of histamine intolerance and are mediated by histamine receptors. These symptoms include:
- Bloating
- Gas
- Abdominal pain
- Reflux
- Nausea
- Vomiting
- Irregular bowels
- Constipation
- Fatigue
- Headaches
- Migraines
- Eczema
- Rash
- Dermatitis
- Hives
- Rhinitis
- Angioedema
Histamine Intolerance: Test
I encourage the mindset that is all about testing for histamine intolerance, and I often promote this mindset when figuring out root causes for issues.
If you test and something is there, it is worth treating and pursuing further.
On the other hand, if it is not there, consider a trial of lowering histamine (in terms of the apparent foods we detailed earlier), and think about things that help stabilize your mast cells.
Since writing this article, some potentially valuable tests have emerged that may help our conversation today. The first is testing for diamine oxidase enzyme activity.
If low, it can be diagnostic, but it could be better as a test. It either misses many with histamine intolerance, or many with symptoms of histamine intolerance have some other underlying issue4.
Critical Insight: The best test to date is likely a skin-prick test. It can accurately identify 79% of those with histamine intolerance5.
While our best bet right now is the skin prick, future new tests may be used to measure the amount of histamine and methylhistamine in urine6.
Also, please do look deep into any hidden infections, gut issues, airborne allergies, food intolerances (Read: The ultimate guide to food intolerances). Those are the more likely culprits and are certainly worth your time.
Bottom Line: If you continually “chase” the diagnosis of histamine intolerance, and it is not measurable in your body, you are playing a losing game. Even if you strongly suspect it, you will never know if you have gotten a handle on it. So, please expand your perspective and try to treat these other issues – they could also be the root cause of your symptoms.
Top 12 Histamine Foods to Avoid
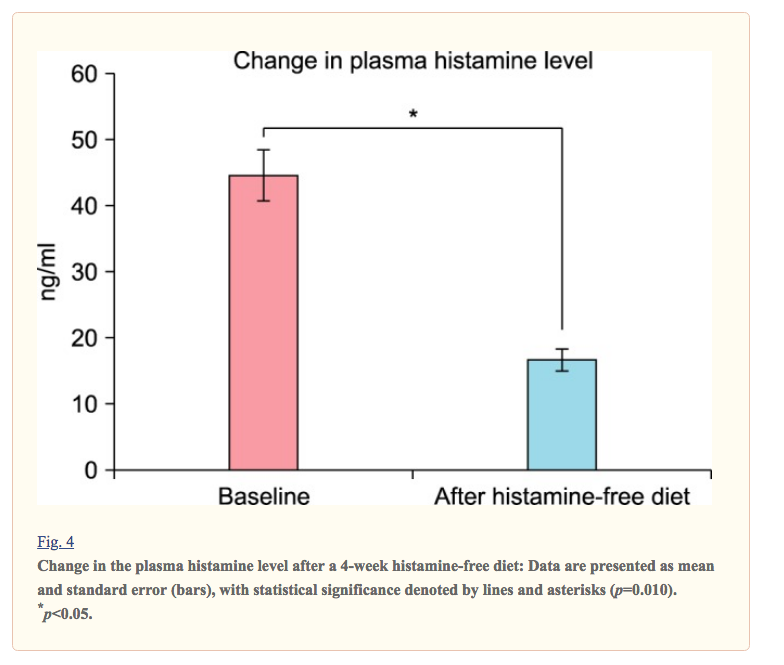
What else did we learn about histamine intolerance in 2023? Low-histamine (not histamine-free) diets can help with chronic urticaria (hives)7.
One study showed that a low-histamine diet, one which could lower urticaria, avoided the following foods:
- Anchovies
- Sausage
- Ham
- Chicken
- Tuna
- Anchovy
- Shrimp
- Miso
- Spinach
- Kimchi
- Cheese
- Seaweed8
The diet lasted four weeks. Symptoms improved, and plasma histamine levels were reduced overall. Lastly, DAO activity did not change.
The final study that I want to highlight surrounds DAO supplements. In a blinded study from 7 hours and 32 minutes to 6 hours 41 minutes – patients noted a reduction in migraines of 1 hour and 24 minutes.
In the study, the placebo reduced the duration of migraines by 54 minutes. While they did help, they reduced migraine duration by 6%9.
Updated Knowledge, Optimized Health
Now that we have learned a little bit more about histamine intolerance, and the latest research surrounding it, I want to help you learn even more about your body.
Please consider taking the Thyroid Quiz (Click Here) today.
It will give you a lot more information than you might have even thought possible and can put you on the right path to leading a healthier life.
1 – https://www.dropbox.com/s/kpkw3itr101e01e/10.1016%40j.aller.2016.04.015.pdf?dl=0
2 – https://www.ncbi.nlm.nih.gov/pubmed/26427614
3 – https://newsroom.heart.org/news/lowgluten-diets-may-be-associated-with-higher-risk-of-type2-diabetes?preview=b2db
4 – https://www.ncbi.nlm.nih.gov/pubmed/29154390
5 – https://www.ncbi.nlm.nih.gov/pubmed/23724226
6 – https://www.ncbi.nlm.nih.gov/pubmed/28715791
7 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5839887/
8 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5839887/#S1
9 – https://www.ncbi.nlm.nih.gov/pubmed/29475774
P.S. Whenever you are ready, here is how I can help you now:
1. Schedule a Thyroid Second Opinion with me, Dr. C, Click Here for Details
2. Need a Personalized Supplement? Check out My Thyroid Specific Formulations
3. Download and use my Favorite Recipes Cookbook Here
4. Check out my podcast Medical Myths, Legends, and Fairytales Here
Dr. C’s gift for figuring out what really works has helped hundreds of thousands of people reverse thyroid disease, lose weight, diabetes, and regain energy. Learn more about the surprising story that started his quest.
P.S. Whenever you are ready, here is how I can help you now:
- Schedule a Thyroid Second Opinion with me, Dr. C, Click Here for Details
- Need help to choose supplements? Click ‘Help Me Decide Here'
- Get my top books Here
Dr. Alan Glen Christianson (Dr. C) is a Naturopathic Endocrinologist and the author of The NY Times bestselling Hormone Healing Cookbook, The Metabolism Reset Diet, and The Thyroid Reset Diet.
Dr. C’s gift for figuring out what works has helped hundreds of thousands reverse thyroid disease, heal their adrenals, and lose weight naturally. Learn more about the surprising story that started his quest.