Reverse T3: Alternative Thyroid Views
Since the early 1990s, there has been another narrative developing about rT3. In this one, rT3 is harmful and causes symptoms by blocking T3 and lowering the basal body temperature.
Blood tests for rT3, T3 or TSH cannot reliably show when it is happening. In this belief system, the only solution is to take high doses of compounded sustained released T3 twice daily.
So where did all the other ideas about rT3 come from?
Please know that I prefer to avoid confrontation. It would be my preference to play nice with everyone, always get along, and have fun. However, there are situations in medicine in which educated and well-intentioned people can put their patients in harm’s way.
This can even happen when their ideas seem intuitive and even when some patients seem to benefit from the approach. That said, I could not respect myself if I did not speak out.
If this were a harmless difference in opinion, I’d be happy to agree to disagree and move on. It is not harmless. People have died from this approach.
My Experience
I had a patient of mine see another doctor and end up on Wilson’s protocol. She ended up spending months in a coma on life support from an overdose of T3. She never recovered from the damage to her brain or her organs.
In another set of cases, I remember seeing a young couple in their 40s who were both on Wilson’s protocol. It seemed to give them more energy at first but now it was no longer working.
They saw me for another opinion on their thyroid care. They were on high doses of T3 for some time and both had severe palpitations. I had them see a cardiologist to make sure they had not sustained damage to their hearts.
It Was Too Late
Both were found to be in late-stage congestive heart failure. Neither had any prior risk factors for cardiac issues. The cardiologist diagnosed their heart failure as being caused by high doses of T3. Even after stopping T3, they still stand to lose from their lifespan.
Sadly, I could give numerous more cases like these.
I first heard about Wilson’s syndrome in the 1990’s while in medical school. The talk at the time was that it was a powerful approach that could help people. In my first year of practice, a patient who was on the protocol from another doctor asked me to take over her care.
She showed me the protocol she was on and explained how she was off to a good start and just needed more medications for her next steps. I read Wilson’s Protocol Doctor’s Manual available at the time and found it intriguing. My eagerness to help led me to believe that this might be a new type of therapy I could use to help others.
I prescribed her an additional supply of the smallest dose available. She had already been on it and I asked her to remain on it while I studied the protocol further. I got an after-hours call that same evening.
The Results
Immediately after starting the new prescription, her heart started racing out of control. It was the same dosage, but I did not know if her next batch was compounded differently or if her body had just had enough. I asked her to stop completely for the time being.
I then read everything I could find, not just the materials from Dr. Wilson. I regret not doing so sooner. What I learned shocked me. Dr. Wilson was no longer practicing because a patient of his died.
The records ascribed her death to a thyroid overdose. I found other stories of patients who had been harmed from this same protocol from doctors Dr. Wilson had trained.
Experiences like this have shaped me into someone who is more cautious and thorough.
The Wilson Model
I harbor no ill will toward Dr. Wilson. I doubt neither his sincerity in his ideas nor his eagerness to help people.
In a perfect world, he would retract his ideas insofar that they do not impune with the known facts about thyroid physiology or clinical outcomes.
I do not expect this to happen and I do believe that some doctors will continue to embrace his ideas despite the mounting evidence. I can only hope that those who are receptive to facts will reconsider.
His work is universally discredited in the endocrinology and thyroid health communities.
However, alternative doctors may find it easy to ignore admonishments from conventional sources. Perhaps since I am far from an outsider to alternative medicine, I will have more of a chance of being heard.
Dr. Broda Barnes
Dr. Wilson’s ideas were largely an extension of those of Dr. Broda Barnes with some elements from the early hypothesis about NTIS. In his words:
“A patient came to my office and she brought with her a book and she said that I should read it. It was called Hypothyroidism: The Unsuspected Illness, by Broda Barnes, MD. In that book, he explains the importance of using body temperature as a guide to evaluate thyroid function.
I was intrigued by that and also his suggested treatment of using desiccated thyroid as an empirical treatment to normalize the body temperature.
Though I did not look at the book for a few weeks, I eventually read it and decided to try his approach in a few of my patients. To my surprise, some of those people got 100% better.
That was really illuminating to me because, according to my training in medical school, that was not supposed to happen.
These people had normal thyroid blood tests and, supposedly, that meant that they could not benefit from thyroid hormone treatment. These people did not get just a little bit better; they got completely better. It did not work for all the patients I tried it with, but it worked in about 60% of cases.
What I Discovered
I was looking at the other 40% and wondering how we could help them, too. It could be that they did not have thyroid problems, or maybe the particular treatment I was using was not really addressing their issue.
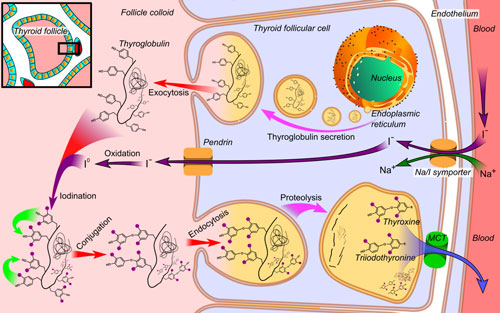
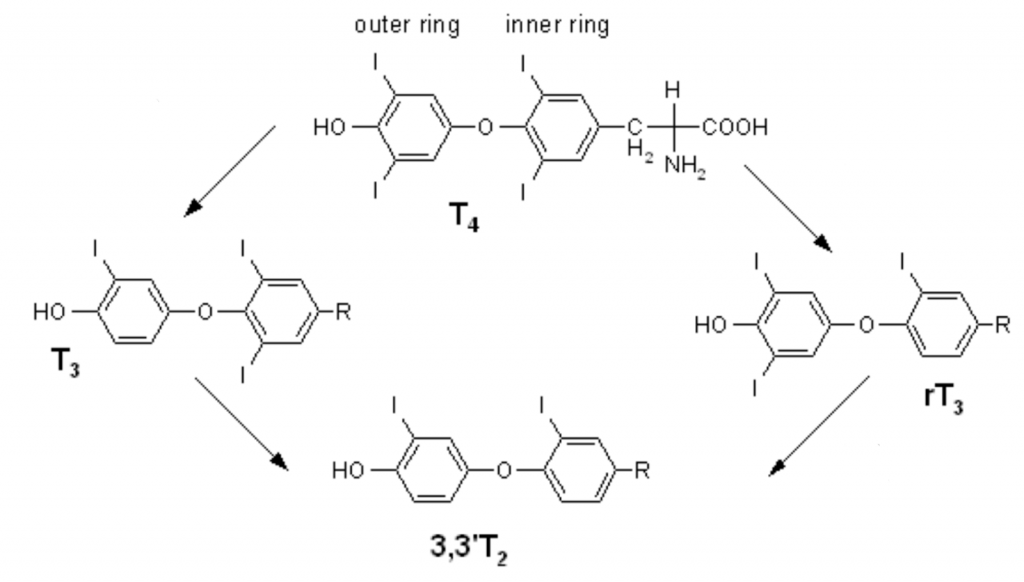
As I was trying to think of ways to increase the yield, I looked at the thyroid hormone pathways and saw that T4 is converted to T3. It turns out that this step is really important.
I thought that, perhaps, these patients have a problem with the conversion of T4 to T3. So I started giving some of these treatment failures—these patients who had failed to respond to the pervious (sp) treatment—T3 directly.
A lot of those treatment failures became treatment successes. That is how it all started.”22
Dr. Broda Barnes and Basal Body Temperature
Dr. Broda Barnes was likely the main source for nearly all dissenting views on conventional thyroid care. In his model, some of his main ideas were:
- Thyroid blood tests were inaccurate
- Symptoms and basal body temperature (BBT) were more reliable tools both for diagnosing thyroid disease and determining the best dose of thyroid replacement
- Natural Desiccated Thyroid (NDT) was superior to synthetic T3 or T4 medication
- Thyroid patients often needed to take hydrocortisone to manage symptoms
The current generation of thyroid blood tests was not available during the course of Dr. Barnes’ practice. Past tests had numerous inaccuracies that gave him valid reasons to be wary. These included:
- Thyroid uptake
- Protein-bound iodine
- Basal metabolic rate
Barnes argued that healthy people should have an axillary (underarm) morning BBT between 97.8F to 98.2F.
If it was lower and they had any symptoms, they needed to take thyroid medicine and increase the dose until their symptoms resolved or until their temperature elevated above 98.2.
Barnes model can be summarized as:
- Axillary temperatures = oral temperatures.
- The thyroid is the prime regulator of BBT.
- BBT should not deviate from 97.8ºF to 98.2ºF.
- The BBT goes up as thyroid doses go up.
- Thyroid doses are safe unless the body temperature elevates.
I will go through these points in some detail because BBT is pivotal to many of the alternative views on rT3. Here is what current research tells us about these points.
Do Axillary Temperatures Equal Oral Temperatures?
No. Strong consensus holds that on average, the axillary temperature is 1º Fahrenheit lower.
In 1990, a study by Agarwal monitored oral and axillary temperatures in 100 patients and found that oral temperature was higher in all cases.
The researchers concluded, “No attempt must be made to extrapolate the axillary to oral temperature.”23
Furthermore, Barnes based the similarity between oral and axillary temperatures on male military recruits. They were inherently younger and more physically active than many populations. They also did not reflect normal temperature variations found in menstruating women.
Data has shown that physically active males have less circadian temperature fluctuation on their axillary temperatures. Their morning readings would, therefore, run higher than morning readings of a less active population24.
Unlike Dr. Barnes, Dr. Wilson recommends taking the temperature orally every three hours or three times daily. He suggests that if the average temperature is below 98.6, Wilson’s Temperature Syndrome is present.
Is The Thyroid The Prime Regulator of BBT?
No. Although the thyroid is a key player in regulating metabolism and temperature, a cascade of other hormones and messenger molecules such as leptin, epinephrine, norepinephrine, and cytokines also play a role.
BBT is governed by many internal and external factors and not just the thyroid gland itself. External factors, such as time of day, season, diet, and lifestyle and internal factors, such as age, fitness, and circadian rhythms play a significant role in temperature variation25.
Is BBT In Healthy Populations Always Within the Range of 97.8 to 98.2?
No. As modern medicine grows toward evidence-based practice, we now understand that there is variability in temperature and that normal temperature occurs within a range of values.
In 2002 a comprehensive review of credible papers on normal human body temperatures from 1935 to 1999 was published. It showed that the range of normal temperatures was from 91.8ºF to 100.6ºF for women and 96.2ºF to 99.9ºF for men.
The conclusion of the meta-analysis was that “The ranges of normal body temperature need to be adjusted, especially for the lower values. When assessing body temperature it is important to take place of measurement and gender into consideration.”26
Does BBT Elevate As Thyroid Doses Increase?
No. In a study of 66 trauma patients, AM axillary temperatures were correlated with TSH, T4, free T4 index, and T3 uptake. Taking account of all the subjects, 86.4% had temperatures below Barnes’s threshold of 97.8ºF.
Of this subgroup, 70% had no abnormal thyroid markers. Of the remaining 13.6 individuals with BBT readings within Barnes’s guidelines, 67% had no abnormal thyroid markers. BBT did not correlate with measured thyroid dysfunction27.
Are thyroid doses safe unless the body temperature elevates?
No. In a study correlating thyroid function with BBT, Ljunggren et al. (1977) found that serum T3 showed a strong inverse relationship with BBT with the lowest levels being present at febrile temperatures of 104ºF. TSH did not correlate with BBT, and reverse T3 showed a nonlinear relationship28.
Barnes’ work has helped many of us realize there is much more to it than that. His work connects us to a time when neither accurate lab values nor biases towards any particular treatment existed. In many of us, he has instilled a spirit of championing patients’ needs over the dogma.
However, with our present knowledge, BBT cannot be safely relied on to prevent hyperthyroid adverse effects of thyroid therapy. The partial truth is that BBT elevates well above normal in cases of thyroid storm29.