Do you have IBS? If you are feeling discomfort, or undergoing tests in hopes of finding an explanation to your digestive symptoms, there could be an easy answer.
Let me help you get to the bottom of your digestive health….




Do you have IBS? If you are feeling discomfort, or undergoing tests in hopes of finding an explanation to your digestive symptoms, there could be an easy answer.
Let me help you get to the bottom of your digestive health….
Product Recommendation: RS Complete benefits GI health through its ability to support microbial balance and proper intestinal permeability and integrity. Additionally, this formula may help support optimal blood sugar and insulin levels, appetite control, and cardiovascular health. Click Here

In a recent article about SIBO, I cited evidence which proved that hydrogen and methane breath tests do not measure SIBO activity. I noted that diets and treatments that strive to reduce bacterial counts are less effective than placebo treatments.
The hypothesis that an overgrowth of bacteria in the small intestine is the cause for digestive symptoms in some people. And, that by reducing these bacteria we can improve their symptoms, is a failed hypothesis. In short, SIBO is not real.
The natural follow up question becomes: what to do for a SIBO diagnosis or ongoing digestive symptoms?
If you were diagnosed with SIBO but do not have digestive symptoms, you do not need to do anything. You can safely disregard the diagnosis, since up to 40% of healthy people will falsely test positive for SIBO.
Researchers made the SIBO hypothesis because they were trying to find a cause behind symptoms like:
In the absence of an explanation, we call these symptoms Irritable Bowel Syndrome (IBS). If we move past SIBO, we can start to identify exactly what constitutes IBS and how you can effectively treat it.
IBS is a combination of abdominal pain, abnormal stools, and bloating. Syndrome, implies that this condition is a collection of symptoms lacking a singular cause.
The first established pattern of symptoms to define IBS was the “Manning criteria,” codified in 1978. It included:
The current symptom pattern used to diagnose IBS is the “Rome criteria.” Four consecutive panels of researchers and gastroenterologists have met to review evidence and update these criteria.
The latest was the Rome IV meeting in May 2016 from which we have the Rome IV criteria. This includes:
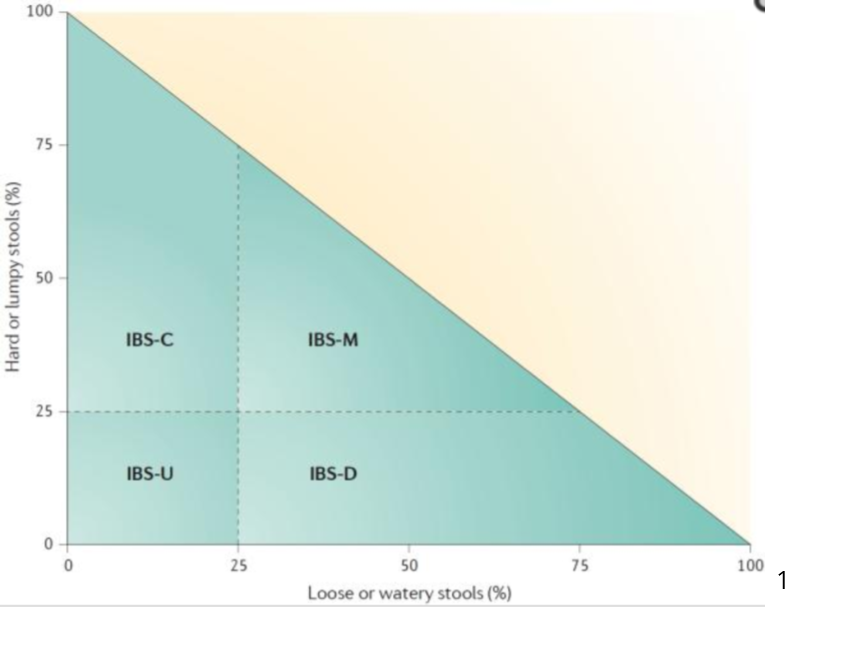
Based on the frequency of hard stools and loose stools, the Rome IV criteria defines the following versions of IBS:
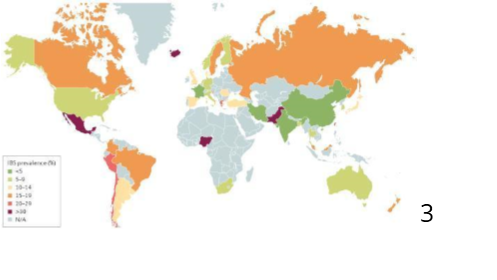
The rates of IBS vary greatly, based on geography.
In some parts of the world, only 1.1% of the population has it.
That said, in other areas it can often be as high a 45%. In the United States and Europe, rates range from 5%–10%.2
Both genders get it, but the condition is more common in women than men. Those who have had early life trauma are also more at risk.
IBS is more common with age, but it is rare for it to first appear after 50 years. 4
There is no clear cause.
Until recently, IBS was categorized as a functional disorder. Unrelated to the term “functional medicine,” functional disorders are defined as conditions in which there is altered function – something does not work right, but there is no apparent change in structure or chemistry.
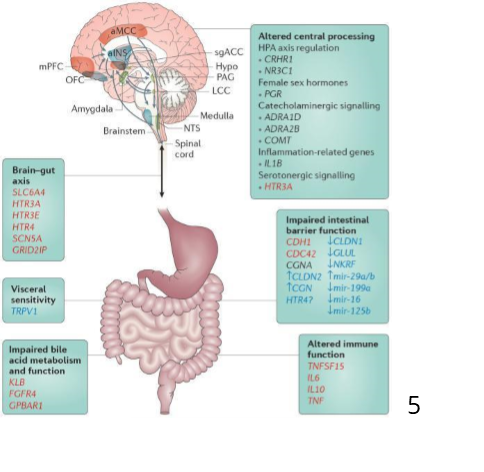
Functional disorders are often stigmatized as being made up or psychosomatic. In 2016 researchers revised IBS from functional disorder to disorder of gut-brain interaction (DGBI.)
Key Insight: Here’s where we run into danger – The concept of IBS as a gut-brain disorder balances on a thin edge. One can easily fall off and construe the idea that IBS is “made up” or “all in your head,” or a function of unbridled hysteria.
Once this problematic view is generally embraced, it seems that one of two paths follow:
Bottom Line: What I want you to know is that IBS (with the exception of PI-IBS) does relate to the brain and the nervous system. It is not made up, it is a very real condition.
Mind-body approaches work not because one is naive or uneducated, but because the brain and the gut connect in powerful ways we are just beginning to understand.
Those who have IBS have higher rates of other functional disorders, also called somatic disorders since they relate to the somatic nervous system – brain and conscious activity. 6

Apart from the Rome IV patterns, another version of IBS is known as post-infectious IBS (PI-IBS). This lasting response happens to about 10% of patients after infectious gastroenteritis.
It seems that inflammation and changes in the nerve activity in the bowels disrupt the flora in ways that lead to lasting symptoms.
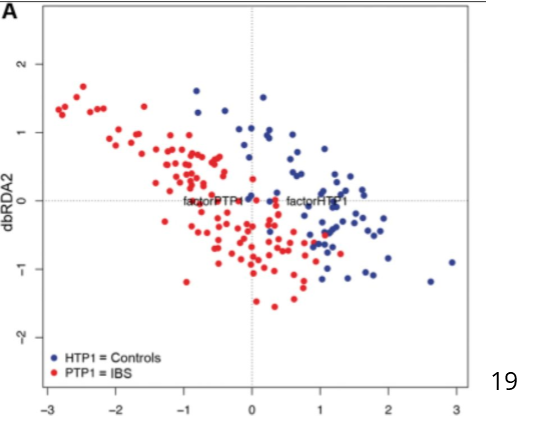
The specific flora changes associated with PI-IBS include:
The changes in flora inhibit the production of short-chain fatty acids. This lack of protective short chain fats, like butyrate, is harmful to the intestines as well as to the whole body.
In PI-IBS the nerves that carry pain signals from the gut to the brain are more active than typical. PI-IBS is also distinct in that it is a structural disease with measurable changes in the intestinal tract. 8
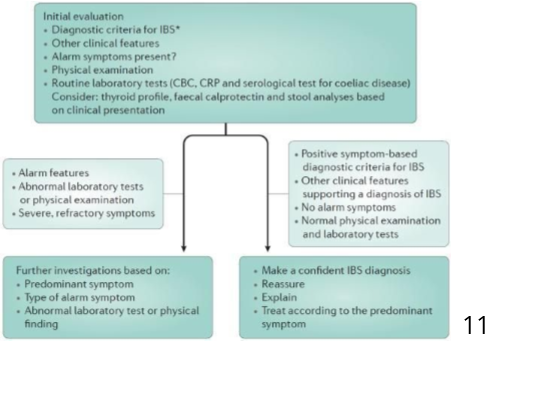
First, one must rule out other causes of digestive symptoms and evaluate for Inflammatory Bowel Disease (IBD) like ulcerative colitis and Crohn’s disease.
Do you happen to have any of these “alarm symptoms”? These include:
History is also a vital component. As it pertains to these symptoms, have you noticed that?
Key Insight: If you have any of these alarm symptoms, it is worth a detailed examination. This can include blood tests, imaging tests, and possibly a visual examination via scope of the upper or lower intestinal tract. Even if you don’t have any alarm symptoms, it is worth following up with the gastroenterologist if you do not have symptoms that fit the room criteria, or you fail to respond to initial treatments.
If you do not have any alarm symptoms there are no specific tests for IBS, although many are in development.
In other cases, routine testing is appropriate to rule out immune diseases, hidden inflammation, thyroid disease, celiac disease, imbalances in the bowel flora, and food allergies.
It is also worth screening for celiac disease because about 1% of the general population has celiac disease. In those that have IBS, the rate is higher, closer to 3%.9
A suggested minimal panel of tests for those who have IBS would include:
If you do have IBS-D or PI-IBS, it is worth having stool cultures to rule out clostridium infections. In the case of IBS-C, it is also important to rule out dyssynergic defecation.
Many people have abnormal nerve responses that tighten their rectum when they attempt to have bowel movements.
This response can lead to many IBS symptoms, but is distinct from IBS.10 If you suspect this condition, most gastroenterologists can diagnose it with a simple physical exam.
For decades, researchers saw an unusual pattern with IBS treatments. Many would work for brief periods of time and then stop.
The more often the participant visited the clinician, the better the treatment worked.
Also, treatments and diets that were based on opposing mechanisms seemed to work equally well.
Key Insight: Given the gut-brain connection, it is impossible to make sense of IBS treatment without acknowledging the placebo effect and its evil twin, the nocebo effect.
Placebo means ‘I please’ and can be a medication, diet, or treatment that has no biological effect, but results in improving symptoms.
As soon as placebo-controlled studies became routine, it seemed that IBS responded to placebos about 50-70% of the time.
In the recent 10-15 years, the rate has dropped off. It seems that participants in studies often connect via social media and are able to figure out before the study is over who is on the placebo and who is not.
Surprisingly placebo treatments also work nearly as well in Inflammatory Bowel Disease as they do in IBS. When it comes to digestive symptoms, placebos do not work better on one gender than another.
There is also no clear pattern with age. Intelligence and educational levels do not predict placebo responses either way.
There is at least one genetic link. Those with catecholamine – o – methyltransferase variations (COMPT) do tend to respond better to placebos.
Something that I feel is understudied is the role of nocebo on digestive symptoms. Nocebo means ‘I harm.’ It seems that those with IBS are more apt to have side effects (nocebo reactions) to placebos than others.12
The interplay between placebos and nocebos can be bizarre. In one study, people with known food allergies were told that they were given an infusion of a low-dose version of the food which causes them to react.
Truthfully, they were given harmless saline, but many had allergic symptoms. During a follow-up procedure, they were given another infusion told that it was an antihistamine and it would block their symptoms. They got better despite the fact that the second infusion was also saline.
It is easy to think of people as gullible, but real changes happen. In another study, those with IBS were given antispasmodic medication which normally acts as a sedative. One group was falsely told that the antispasmodic was a stimulant. Not only did this group have stimulant side effects like anxiety and a racing heart, they had lower blood levels of the medication than those who were told what it really was.
I remember one of my first forays into natural medicine. It was a book that claimed that combining carbohydrates and proteins in one meal would lead to digestive distress and eventual poor health.
Once I was enlightened about this effect, I noticed that I felt genuinely unwell when I did not heed the advice. I experienced a nocebo reaction. I now understand how digestion works and know that there is no truth behind this claim.
This first step put me on a path of fear and unease. I read countless books and the more possible reactions I learned about, the more I seemed to suffer from.
Often the diets I followed were far too restrictive in calories and nutrients for a physically active young man.
As my health declined I went into a spiral of fatigue, depression, and paranoia about food. It was only years later that I realized that these symptoms were not present until I expected them to be.
At the low point of that journey, I contorted my life to abide by numerous, contradictory rules in hopes of feeling better I.
During this process I attended college on a full-time basis, studying pre-medical sciences and worked over 30 hours per week to pay for my school and expenses.
The irony is that the best paying job I could find was that as a waiter in a pizza restaurant. I spent each moment of every shift in constant loathing of the ‘bad’ food around me and in judgment of the ignorant souls who ate it.
If that’s not enough of a perfect storm, I was also running about 5-10 miles each day outdoors in Northern Minnesota.
In case you didn’t know, raw salads do not help you adapt to -40 temperatures. My weight kept dropping, I was miserable, and my food cravings were off the charts.
The books I read convinced me that I was clearly toxic. I must have been losing weight because my gut was toxic, and I wasn’t absorbing nutrients. The cravings were clear signs that something I was eating was setting me off. If only I could clean myself out better, then everything would fall into place.
I’ve seen far too many people fall into the same trap. I think that at some point the dietary restriction leads to a real compromise in the capacity of the digestive tract. One can go from fear of foods and an exaggerated experience of symptoms to a place where malnourishment leads to damage.
Bottom Line: The crazy counterintuitive truth is that diets don’t help IBS. Let’s be clear. When I got going on my journey, it was clear that changing my diet completely improved my digestion. You may have experienced the same thing or no doubt you’ve heard others with similar experiences.
There are those with undiagnosed celiac disease, or food allergies. Those are different stories. For those without clear food reactions – many people who change their diets do feel that their digestion improves.
It seems that diets help and for many, they do – at least for a while.
To date, no diet has helped IBS better than placebos.13
It seems so intuitive that if you have digestive symptoms, it must be caused by what you ate. Especially when symptoms often come on in short periods of time after meals and are often much better long periods of time after eating.
Let’s think about a car analogy for a moment.
There are scenarios in which poor quality gas that makes the car run badly. Yet there are also nearly limitless ways the car can go wrong that have nothing to do with the quality of the gas.
If a car has a problem with its electrical system, it would seem to only be a problem when the car was running. You’d never notice any issues when it was shut off. So too it is with the digestive system. If something is wrong, you would be less likely to notice anything when it was not busy digesting food even if the food were not the culprit.
If you are lucky enough to have found that one of these diets has given you lasting relief from IBS. Please don’t change. The question I’m trying to answer is – for those who have not yet found relief, what is most likely to work with the least trial and error.
Here are some of the food choices that I recommend, which may consistently help with IBS:
Here are other things you might want to consider for IBS treatment:
According to one particular study, butyric acid was shown to have powerful anti-inflammatory effects on the body. This means that butyrate can provide benefit when it comes to hypersensitivity on intestinal receptors, as is the case with IBS.20
Key Insight: What’s the best way to raise butyrate? Some have proposed butter as a source. Butter does have butyrate, thus the similar name. Butyrate is also responsible for the flavor in butter. However, the amounts found in butter are far too low to be helpful.
Butter typically consists of 3 – 4% butyrate by weight.21 If you had a teaspoon of butter, weighing about 5 grams, you would have roughly 150 mg of butyrate.
Butyrate is powerful when the bacteria in your colon makes it, but much less when you take it. This is because it changes on the way down, and loses nearly all of its potency. Studies using this method found that 8000 mg was needed to show a clinical change in the colon flora.22
That means that if you were to use butter to try and change your flora, you would need about 1.1 cups of butter, several times each day – which amounts to about 5300 calories!
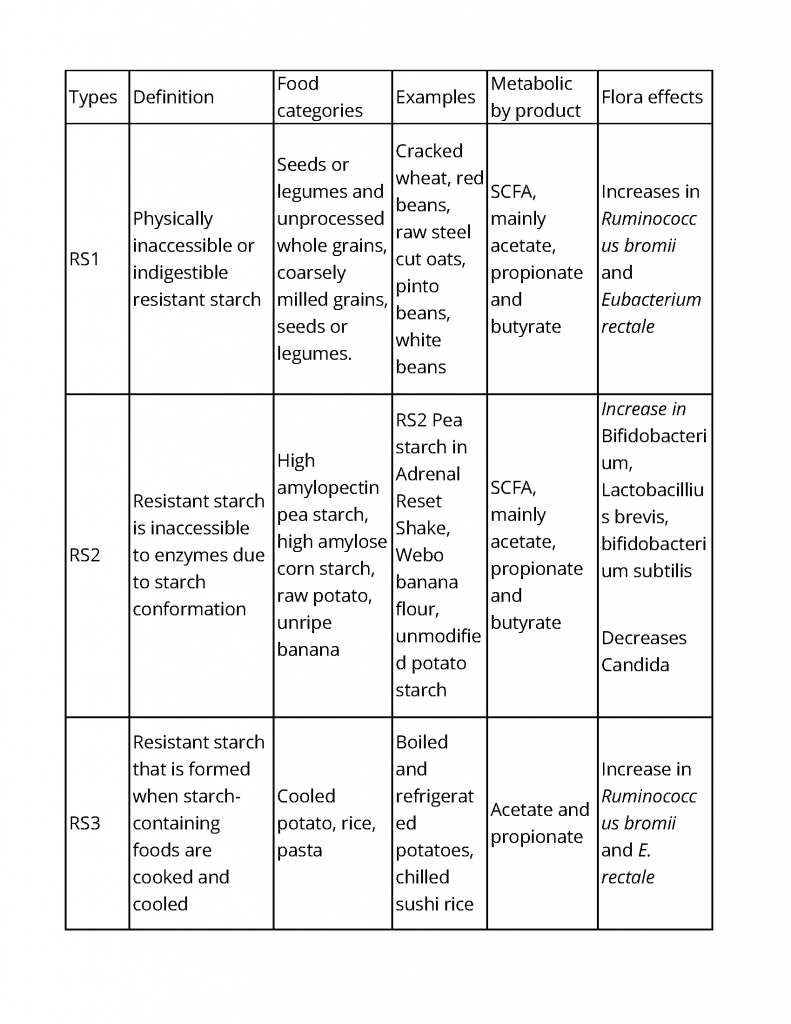
A much more efficient way of raising your butyrate levels is with resistant starch (RS) (Read: Don’t resist this starch). In a recent human study, just seven days of a diet high in RS was shown to improve butyrate levels and increase many strains of protective bacteria. These results kept increasing for a full week after the RS was stopped.
There are distinct types of resistant starch, which you can see illustrated in the chart below:
Now let’s get back to considering some of the other treatments for IBS…
Bottom Line: There are many approaches that deal with handling IBS and it’s symptoms. The best thing you can do is to find what works for you, like introducing more resistant starch into your diet, and taking things one day at a time to get your health (and your life) back in order.
There are certain medications which may be useful when it comes to the treatment of IBS. You have…
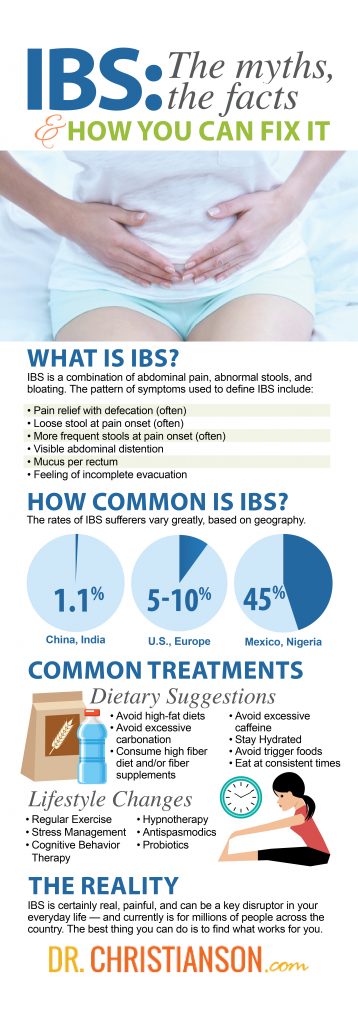
IBS is certainly real, painful, and can be a key disruptor in your everyday life – and currently is for millions of people across the country.
The most effective treatments include natural compounds like resistant starch, peppermint oil, and s. cervasie, and perilla, mind-body approaches like hypnotherapy, CBT, and yoga are also of value.
Fiber is useful on a long-term basis, but must be adjusted slowly.
I hope you have learned a little bit more about IBS today, and how you can use this important information moving forward.
Want to expand the knowledge of your own health even further? Please feel free to take the Thyroid Quiz (Click Here) today, and gain a deeper understanding of your own personal health.
1 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5001845/
2 – https://www.ncbi.nlm.nih.gov/pubmed/28885302
3 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5001845/
4 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5001845/
5 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5001845/
6 – https://www.ncbi.nlm.nih.gov/pubmed/17900326
7 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5001845/
8 – https://www.ncbi.nlm.nih.gov/pubmed/28885302
9 – https://www.ncbi.nlm.nih.gov/pubmed/27753436
10 – https://www.iffgd.org/lower-gi-disorders/dyssynergic-defecation.html
11 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5001845/
12 – https://www.ncbi.nlm.nih.gov/m/pubmed/18095162/?i=9&from=irritable%20nocebo
13 – https://www.ncbi.nlm.nih.gov/pubmed/28440580
14 – https://www.ncbi.nlm.nih.gov/pubmed/17488254
15 – https://www.ncbi.nlm.nih.gov/pubmed/25070054
16 – https://bmccomplementalternmed.biomedcentral.com/articles/10.1186/1472-6882-14-173
17 – https://www.ncbi.nlm.nih.gov/pubmed/29372567
18 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5236513/
19 – https://www.ncbi.nlm.nih.gov/pubmed/26239401
20 – Banasiewicz T, Kaczmarek E, Maik J, et al. Quality of life and the clinical symptoms at the patients with irritable bowel syndrome treated complementary with protected sodium butyrate. Gastroenterol Prakt. 2011;5:45–53.
21 – https://www.sciencedirect.com/science/article/pii/S0304394016300775
22 – https://onlinelibrary.wiley.com/doi/10.1046/j.1365-2672.2002.01679.x/full
23 – https://www.ncbi.nlm.nih.gov/pubmed/27112106
24 – https://www.ncbi.nlm.nih.gov/pubmed/21691341
25 – https://www.ncbi.nlm.nih.gov/pubmed/24935275
26 – https://www.ncbi.nlm.nih.gov/pubmed/25858661
27 – https://www.ncbi.nlm.nih.gov/pubmed/3306904
28 – https://www.ncbi.nlm.nih.gov/pubmed/25224525
P.S. Whenever you are ready, here is how I can help you now:
Dr. Alan Glen Christianson (Dr. C) is a Naturopathic Endocrinologist and the author of The NY Times bestselling Hormone Healing Cookbook, The Metabolism Reset Diet, and The Thyroid Reset Diet.
Dr. C’s gift for figuring out what works has helped hundreds of thousands reverse thyroid disease, heal their adrenals, and lose weight naturally. Learn more about the surprising story that started his quest.