Did you know that iron can be the key to your health? It’s important to know how good it can be, what are the right amounts, and what you can do to get more of it at the right time.
- Have any questions?
- 480-631-7837
- support@in-goodhealth.com

Podcast – Does Red Meat Cause Cancer? with Dr. Garth Davis
May 11, 2020
Podcast – Does Animal Protein Cause Cancer? with Dr. Gabrielle Lyon
June 8, 2020
Podcast – Does Red Meat Cause Cancer? with Dr. Garth Davis
May 11, 2020
Podcast – Does Animal Protein Cause Cancer? with Dr. Gabrielle Lyon
June 8, 2020Home > Hormone Reset > A Deep Dive On Iron
A Deep Dive On Iron

Now let’s get into the topic at hand: iron! Learn about iron and what it does for your body by reading our guide.
Iron: The Basics
By now, you may know all about the more stubborn symptoms that go along with thyroid disease (Read More: The Complete Guide To Testing Your Thyroid). These include just some of the following:
- Fatigue
- Hair Loss
- Insomnia
- Brain Fog
The problem is that these symptoms may not improve with thyroid medications. Or, only with an overdose of these medications (which we would also want to avoid).
I often hear about iron being discussed as a way to manage these symptoms, but is that true? At the same time, we often hear about iron being spoken about as a danger and something to be avoided.
For those with thyroid disease, it is especially important to work with a doctor who knows the requisite iron you need.
Key Insight: The important thing to know is that iron can be treated and your symptoms can improve. Today, I’ll explore more about this concept and how it can potentially change your life.
Iron: Defined
At any given point in time, the adult human body contains about 4-5 grams of iron. Around 65% of this is in the form of hemoglobin — the remainder is mostly stored in the liver, in the form known as ferritin.
Iron is helpful because it is such a reactive element. Its main role in the body involves the movement and use of oxygen, which is essential!
Iron & Your Thyroid
So, what’s the connection between iron and your thyroid?
If we break it down, iron is made into what we call heme proteins. These include thyroid peroxidase (TPO), which is needed to bring iodine into the thyroid to make hormones.
When you are lacking in iron, your thyroid hormones may not be produced in large enough quantities. They may also not be able to work correctly in the cells themselves.
At the same time, the relationship is shared. If thyroid hormones are too low or too high, it can be harder for the body to regulate iron. They have an effect on one another.
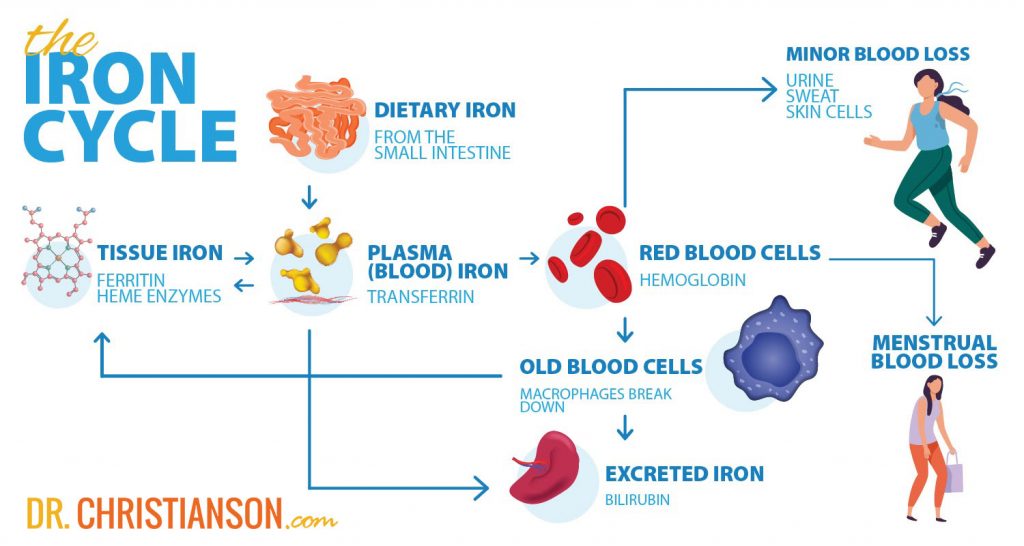
The Cycle of Iron
What happens to iron when it enters the body? How does it enter in the first place?
Iron enters the body from the diet. It is absorbed in the small intestine, and how much iron we absorb from there is based on just how much we need.
The more we have, the less we absorb, and vice versa. While this is true, there are some limits to how much we can absorb. In a best-case scenario, only a few milligrams are absorbed per day (even if high amounts come in from the diet or supplements).
After being absorbed, iron quickly goes into storage or into the production of red blood cells (which live about 120 days). After dying, their iron is stored for reuse or eliminated in our stool.
Key Insight: Some iron is also lost from menstrual blood and directly from the plasmas.
Men, and non-menstruating women, lose about 1 mg of iron per day in their stools. If a woman is menstruating, she is losing an additional 20-60 mg of iron per cycle (making their daily iron loss higher).
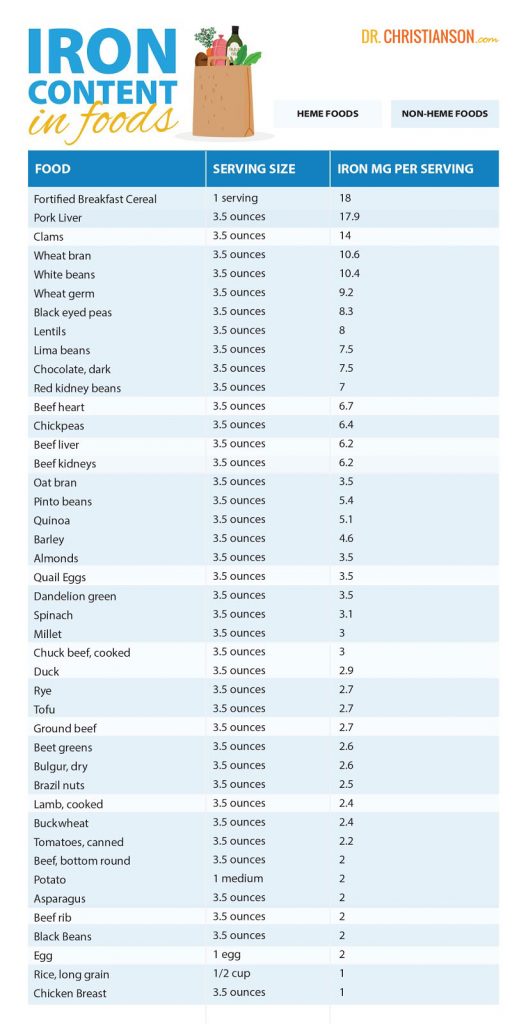
Iron In Our Diets
The iron that we get from our diets comes in two distinct forms:
- Heme Iron
- Non-Heme Iron
Foods that come from animals have both, whereas plant foods only have non-heme iron.
We can only absorb 2-20% of non-heme iron and 15-35% of heme iron. That said, things like vitamin C are able to improve iron absorption.
Key Insight: Average diets that contain vitamin C, heme, and non-heme iron net around 14-18% absorption — vegetarian diets, on the other hand, average 5-12%.
It turns out, though, that our bodies are more flexible as it pertains to the absorption of non-heme iron. When we need more, and when we need less, we can absorb it accordingly.
Let’s consider this example. If a menstruating woman needs around 3 mg of iron every day, and she absorbs 15% of it, she would need 20 mg of iron in her diet. If she only absorbed 5%, though, she would need 60 mg per day.
The same thought process applies to vegetarians who may need to be more mindful of their iron intake. That said, they do have a lot of good options available to them.
As you’ll see below, the problems with iron deficiency have more to do with large amounts of iron debt that slows our overall rate of absorption.
If things are working well and everything is firing, dietary iron can work perfectly well. That said, they often cannot prevent a deficiency and rarely can correct one.
Iron Absorption In The Body
Now that you know more about the iron you can find in common foods, it’s important to realize and consider the context of a meal and its effect on iron absorption.
Let’s break each of these essential elements down:
Phytates
Most plant foods contain naturally-occurring compounds that we call phytates. These compounds may have numerous health benefits such as immune enhancement cancer protection, cholesterol reduction, and prevention of calcification1.
Phytates are lowered in foods due to processing grains, fermentation, and soaking. They also have less of an effect on iron absorption if they are paired with a source of animal protein.
Polyphenols
These are antioxidants that can be found in many plant foods and beverages. They also have a binding effect on iron, and foods with enough of these to be relevant include teas, chili, and wine. If consumed apart from meals, though, the effect may be reduced.
Calcium
Although the data is mixed, calcium may not have negative effects on heme iron (but it does have a negative effect on non-heme iron). Those who consume calcium-dense foods, or supplements, alongside mixed meals do not have an issue maintaining iron status.
Those that are low in iron are often advised to take iron-rich foods, or supplements, apart from dairy foods or insoluble calcium supplements (which includes calcium carbonate, oyster shell, coral, or algae-derived sources).
Protein
When it comes to iron absorption, it all depends on the type of protein you’re consuming (Read More: How Much Protein Is Best For Weight Loss?).
Animal-tissue protein, from poultry, pork, or beef seems to enhance the absorption of nonheme iron. But, animal protein from milk or eggs may inhibit iron protein.
Vitamin C
No matter how you’re getting it, whether from food or supplements, vitamin C improves the absorption of iron and lowers the negative effects of things like phytate, polyphenols, and even calcium!
The Symptoms of Iron Deficiency
All is well so long as the amount of iron absorbed by your iron keeps up with the amount you are losing. That said, if too little is absorbed, or too much is lost, a deficiency emerges.
If you are lacking in iron, oxygen cannot be utilized as well, essential proteins cannot be made, and many enzymes are simply not produced.
All these shortcomings can produce countless symptoms, including:
- Fatigue
- Hair loss
- Poor hair growth
- Poor immune system
- Shortness of breath
- Cold hands and feet
- Anxiety
- Panic attacks
- Leg cramps
- Feeling cold
- Feeling tired, dizzy, and weak
- Memory loss
- Depression
- Heavy menstrual cycles (both a cause and a symptom)
- Shortness of breath and a rapid heartbeat, even when resting
- Joint pain
- Muscular pain from minimal exercise
- Insomnia
- Headaches and migraines
- Craving of ice chips
Conditions Associated With Iron Status
So, what are some of the most and least common conditions associated with iron status? Let’s break them down for you so you can know what to look out for starting today…
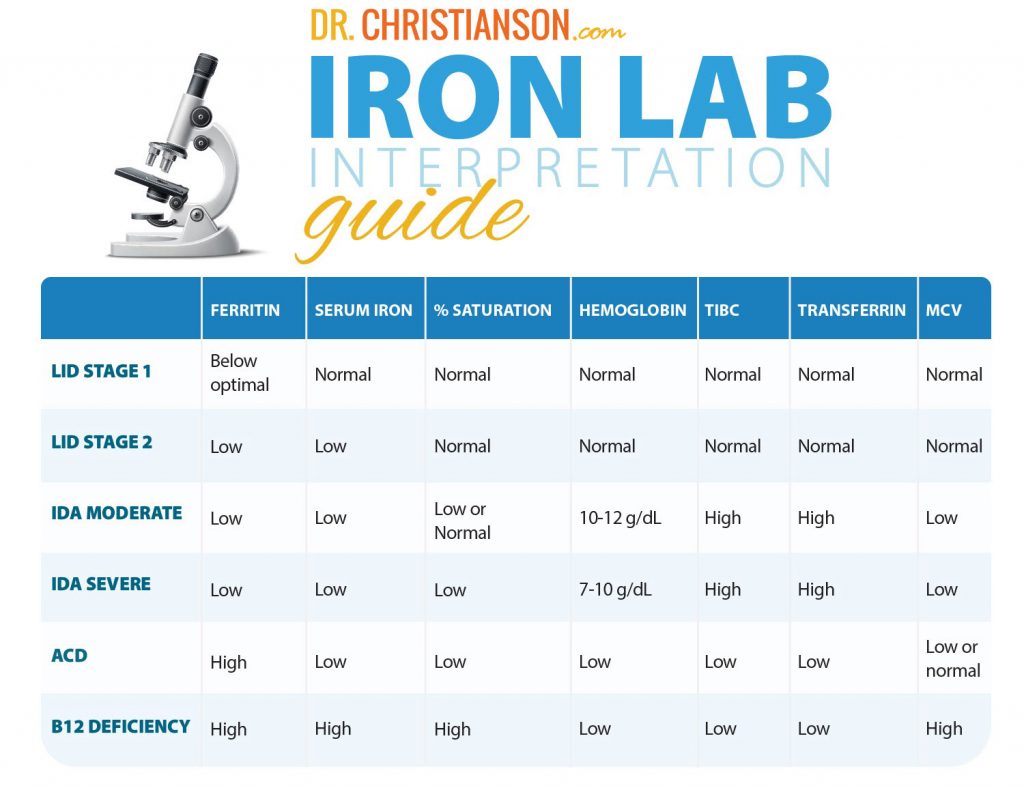
The most common is what we call latent iron deficiency (LID), otherwise known as iron depletion. In fact, this condition may be three times as common as iron deficiency anemia (IDA).
Key Insight: In many cases, untreated iron depletion can ultimately lead to iron deficiency anemia.
Let’s break down the steps in the process:
- Depletion of iron stores in the body
- Iron deficiency without anemia
- Iron deficiency anemia
Bottom Line: There are other types and symptoms involved with anemia, but it is always important to know that you will want your doctor’s guidance when it comes to treating and dealing with anemia.
Can You Get Too Much Iron?
It is possible to get too much iron, in what we call iron overload. That said, it is rarely a problem unless someone is genetically prone to getting it.
The common advice is that it is best not to take iron unless you know you need it, because genetically some are prone to store too much. Even when stores are full, the body may not lower the overall absorption.
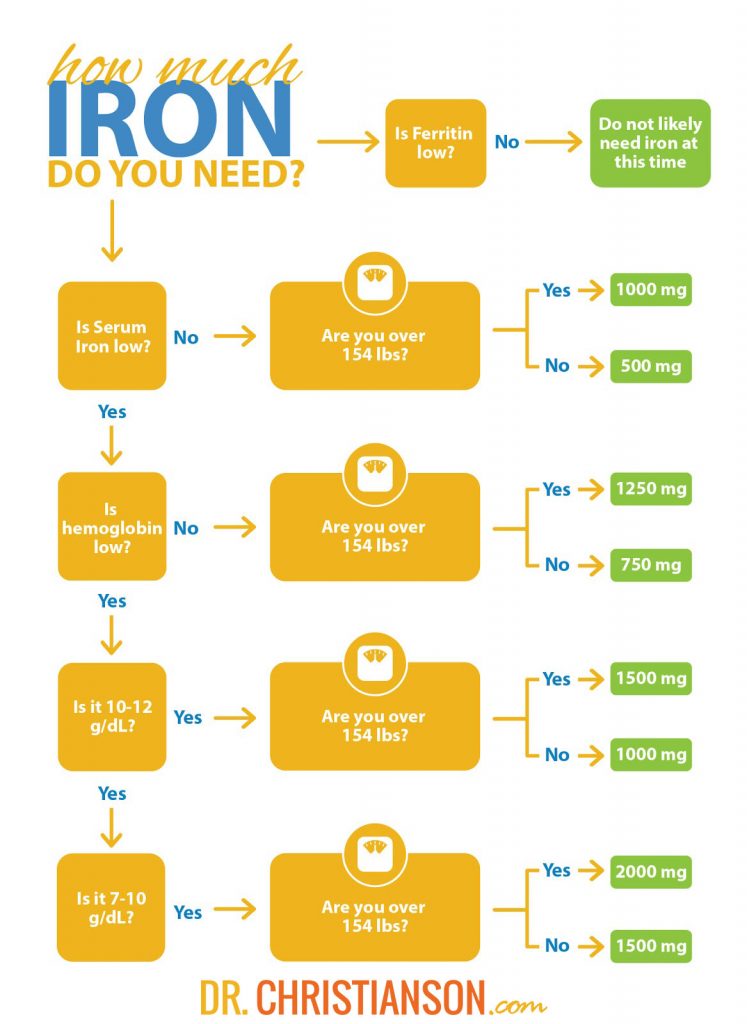
Testing For Iron

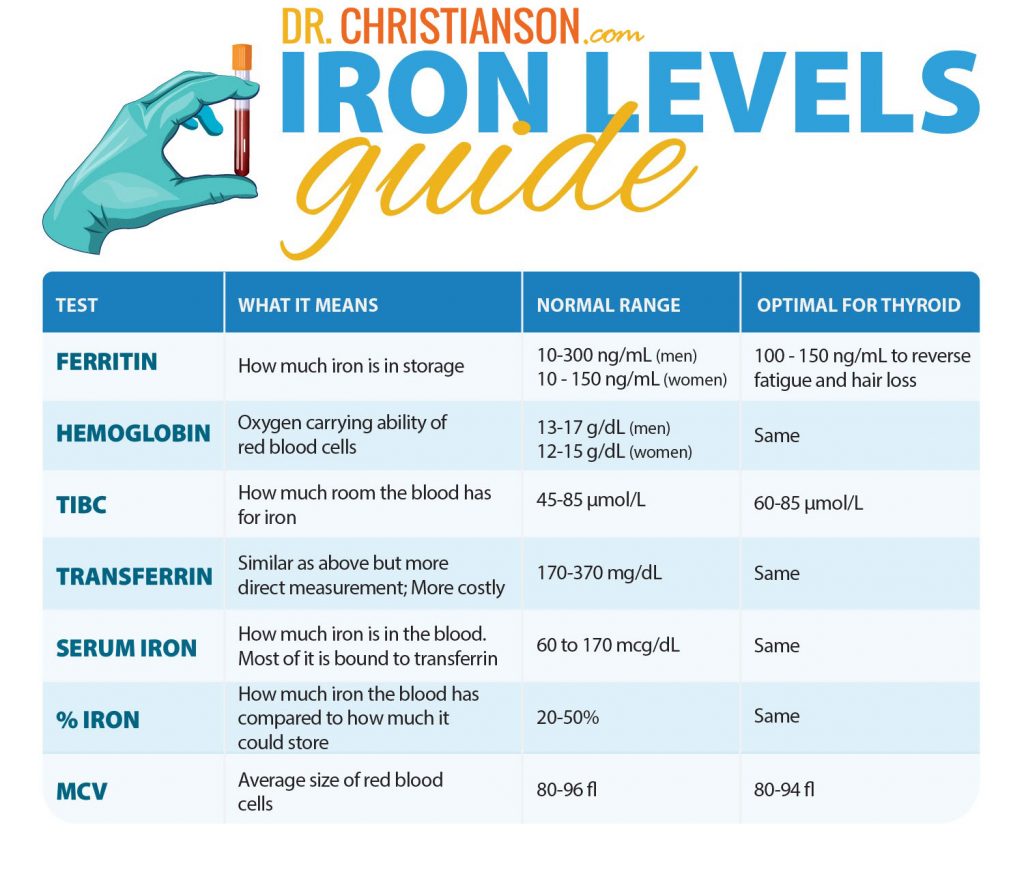
Now, it is important to get a comprehensive idea of the testing that goes into assessing your iron status. I want to begin this part of the discussion by introducing some helpful terms for you:
- Ferritin – The iron you have in storage
- Hemoglobin – Oxygen-carrying molecules in red blood cells
- Red Blood Cells – Use hemoglobin to carry oxygen in the body
- Bone Marrow – Forms red blood cells, white blood cells, and platelets
- Serum Iron – Iron you have in storage
- MCV – Mean Cell Volume, the average size of your red blood cells
- Transferrin – The protein that carries iron
Key Insight: Ferritin can sometimes be misleading in cases of recent supplementation, acute illness, recent hard exertion, and other reasons.
What Blood Levels of Ferritin are Best?
When it comes to ferritin, the normal range is between 10 – 190 ng/mL . If you are under 30 ng/mL, you may be at high risk for latent iron deficiency, and lower than 10 ng/mL is a high risk for iron deficiency anemia.
If you have thyroid disease, you may need your ferritin to be over 100 to reverse latent iron deficiency symptoms currently present2.
That said, here is a helpful chart with the levels you need to know:
Retesting and Tracking Iron Levels
You should start with a retest in 4-6 weeks, followed by a retest in 12 weeks if things are not improving. If things continue to not improve, change your therapy and retest in 4-6 weeks.
Key Insight: The important thing to know is that you should keep monitoring your iron levels, because many people do not need it long term.
What Are Common Causes For Iron Deficiency?
There are some common causes that we might want to consider when it comes to latent iron deficiency, iron deficiency anemia, or anemia chronic disease:
- Low intake of iron
- Low heme iron diet
- Vegan or vegetarian
- Malabsorption
- Autoimmune gastritis
- Caffeine
- Celiac disease
- H.pylori
- Inflammatory bowel disease
- Low intake of vitamin C
- Iron loss
- Endurance exercise
- Heavy menstrual cycles
- Hidden colorectal cancer
Iron Deficiency Anemia and Thyroid
In general, hyperthyroidism leads to low ferritin, hypothyroidism, high T3, high T4, and all lower serum ferritin3.
Iron deficiency also decreases serum T4 and T3 concentrations, in addition to peripheral conversion of T4 to T3 (decreasing T3 metabolism).
If you work on correcting iron deficiency anemia, you can:
- Improve your basal body temperature
- Lower your TSH
- Lower your rT3
- Raise your fT3 and fT44
Bottom Line: A certain type of anemia, macrocytic anemia, occurs 20 times more frequently in patients with hypothyroidism — and found in up to 55% of patients with hypothyroidism5,6,7.
Risk Factors for Anemia
It is important to know that iron deficiency is common in children and adolescents, as well as relatively common in elderly populations.
Moreover, women of childbearing age are most at risk of a deficiency due to losses in menstruating and pregnancy. In general, iron deficiency may be an often unrecognized cause of fatigue in pregnant women.
For men, gastrointestinal conditions are typically the primary cause of iron deficiency anemia.
Obesity is also a risk factor. This may be due to the reduced absorption of iron from the upper gastrointestinal tract, increased requirements, and the impact of obesity-related inflammation in the body.
Then, there are endurance athletes. Because of the broad range of what we consider “normal” for ferritin levels, those who are undergoing high levels of exercise may need more to avoid a deficiency in their body.
Last, but not least, are the special needs required during pregnancy. Adequate supplementation can prevent complications of severe anemia.
When Should You Suspect Malabsorption?
If you are curious whether or not malabsorption is something you are dealing with, there are some common signs to keep in mind:
- Dealing with recurrent anemia
- Low in other nutrients (like zinc and B12)
- Significant gastrointestinal side effects from oral iron pills
- No change even after 6 months with oral iron pills
The most common causes of malabsorption include things like celiac disease, gastric bypass surgery, inflammatory bowel disease8, and H.pylori9.
Understanding H.pylori
In the United States alone, around 30-40% of adults have H.pylori10.
Screening for it can be a helpful step for those already dealing with thyroid disease that are also encountering:
- Acid reflux/heartburn
- Recurrent iron malabsorption
- Inability to normalize thyroid levels
As an initial form of screening, blood tests can be used for H.pylori. Breath tests can also be more definitive, or even a pill that can help determine if the condition is present.
Key Insight: The gold standard, though, is a biopsy done of the stomach.
Treating H.Pylori
Once you know whether or not you have it, there are some useful treatment regimens to consider (with combination antibiotics), including the following:
- Amoxicillin
- Tetracycline
- Metronidazole
- Clarithromycin
In addition to one of the following:
- Ranitidine bismuth citrate
- Bismuth subsalicylate
- Proton pump inhibitor
Natural Alternatives for H.Pylori
The following have had some research on their efficacy against H.pylori:
- Garlic
- Green Tea
- Red Wine
- Broccoli Sprouts
- Licorice
- Honey/Propolis
- Probiotics
Key Insight: While they have all had some partial effects against H.pylori in test tube studies, none have been consistently effective against the infection in humans11.
There are a total of eight protocols that the FDA has approved as being effective. Multiple options exist in cases of the bacteria being resistant or individual intolerances to particular medications12.
Once someone has been treated, blood tests will not show whether or not the treatment worked for months or years. In this case the breath test or stool tests are better options.
Does H.Pylori Cause Autoimmune Thyroid Disease?
H. Pylori infection has been considered a causal link for several endocrine diseases including obesity, parathyroid disease, diabetes, and osteoporosis, although none of these correlations are clear13.
There has been mixed data, some studies showing that treating H pylori lowers thyroid antibodies and others showing it does not and that it does not predict thyroid disease14,15,16.
The strongest evidence linking the two conditions suggests only a weak connection in a population with high rates of H.pylori.
I’m writing about this concept in immunology not because it opens up any current treatment options but rather to draw question to the claim that thyroid patients are benefitted by identifying and eradicating high prevalence possibly commensural infection such as H pylori and Blastocystis hominis.
It is possible that the effects that H pylori would have on adults with existing thyroid disease could be different than its effects on the risk of children developing thyroid disease.
Nonetheless, the evidence of infections like H pylori lowering the risks for thyroid disease are a clear example how in the absence of strong evidence, speculation can lead to conclusions that are not only incorrect but exactly opposite of the findings that come from human studies.
Autoimmune gastritis
Autoimmune gastritis (AIG) is a condition in which the normal functions of the immune system are mistakenly targeted against the stomach lining. This immune attack leads to chronic inflammation and damage to the cells involved with absorbing nutrients. Some of the more difficult to absorb nutrients are the first to show clear signs of deficiency. These include iron, B12, folate, and zinc.
Autoimmune gastritis is a common cause for nutrient malabsorption in the population in general and it is even a more prevalent risk in those with thyroid disease.
As many as 35% of people with autoimmune thyroid disease may also have autoimmune gastritis12. But also other autoimmune diseases such as diabetes type I, Addison’s disease, and vitiligo, also show an increased risk3,4.
Diagnosis
The diagnosis can be tricky because most people with autoimmune gastritis do not have any symptoms. Some studies of general populations showed that when those undergoing routine annual checkups were screened for autoimmune gastritis,
19.5 % were found to have positive antibodies attacking their stomach’s parietal cells. These numbers got higher as they looked at older age groups and those with Helicobacter pylori infections5.
The condition can be screened for with blood tests including blood levels of parietal cell antibodies (PCA) and gastrin. If these levels are unusual, it is appropriate to follow up with an evaluation of the stomach and esophagus with an endoscope. This process is important to be clear on the diagnosis and also to determine if damage has already taken place.
The main risk for undiagnosed AIG is esophageal or stomach cancer. The ongoing inflammation from the immune system’s attack increases the risk of abnormal cell growth.
AIG should be considered in anyone with unexplained anemia or upper intestinal symptoms like heartburn, gas or bloating. In those who have it, dietary changes and even supplements are often not effective at correcting nutrient deficiencies. In these cases it is more effective to give intramuscular (shots) of B-12 or folate when they are low, and intravenous doses of iron or zinc when they are deficient8.
Treatment
There is no direct treatment for AIG. those who have it need to be closely monitored to make sure they have adequate amounts of nutrients and to make sure they have not developed cancer of the upper intestinal tract9.
Raising Iron Levels
Diet and Supplements
Topical
I’ll mention topical iron supplements only toward the interest of making this post comprehensive. They are not common products and there is no reason to think they work. If you do see topical iron available, please don’t consider it a viable option.
Oral
Iron pills come in a variety of forms and potencies. Regardless of the type, a therapeutic dose is 60-200 mg of iron daily. The main limit of iron supplements is gastrointestinal side effects. The majority of people experience some combination of discomfort, bloating, or constipation while taking iron. Dark stools can also be noticed as a normal side effect.
Forms of iron include:
- Iron bisglycinate
- Heme iron
- Ferrous iron like ferrous sulfate, ferrous fumarate, and ferrous gluconate
- Ferrous glycinate sulfate
- Iron protein succinylate
- Ferric citrate
Many forms of iron that claim to be gentler on the stomach are generally just much lower in potency. A low potency dose of iron will likely be better tolerated but it will not likely improve iron levels.
Of the various forms, I recommend Iron bisglycinate for the best combination of absorption, tolerability, and cost-effectiveness.
Iron timing
It turns out that taking iron every other day may be better.
Studies have shown that iron absorption depends on the activity of a carrier protein called hesperidin. This protein may take more than a day to completely unload the iron into the bloodstreamblood stream.
Those who take a dose on alternating days likely absorb as much as those who take iron one or twice daily. Even more dramatic is their reduction of side effects. REF
I encourage adults who need iron to take their full dose on alternating days only and 1 hour before meals. With our iron chelate product, this translates into 3 – 6 capsules in a single dose every other day away from food. Please do not take it at the same time you take your thyroid medication. Take it at least 4 hours later.
When iron pills work well, you may build up your iron stores by 5 -15 mg daily.
You should allow this long for symptoms to improve and before needing to retest.
Infusions
The final version of iron is iron infusions, also called iron IVs.
The drawbacks of iron IVs are that they have a substantial rate of side effects, including anaphylaxis, and they are not always properly administered, especially by IV bars or elective nutrient IV centers.
The two main types of iron IVs are:
- Iron detran
- Iron sucrose
The older version of iron detran did have a significant risk of allergic reaction. With iron sucrose, this risk is lower.
It also helps to be mindful of side effects, in general, that you may encounter when you receive an IV. This might include:
- Flushing
- HA
- Dizziness
- Nausea
- Anaphylaxis-especially with iron detran
Typically, you would receive an IV infusion 2-5 times over 1-2 weeks. If needed, you may also need another over the course of a year (often somewhere between 1-2).
What About Iron Supplementation During Pregnancy?
If you are pregnant, it definitely helps to have a better understanding of iron during this time. One study I came across noted that IV treatment helped restore iron stores faster and more effectively than iron taken orally (with no adverse reactions).
Should I Consider A Blood Transfusion?
It is important to know that a transfusion may only be necessary in serious cases of iron deficiency anemia (wherein one is not responsive to an IV).
This is generally secondary to a case of major blood loss post-surgery or in some form of trauma.
How Quickly Can You Raise Your Iron?
Once you know how much iron you need, you can quickly determine how long it should take to build it up.
This is important to consider because symptoms may not improve until you fill your stores back up. Say you have hair loss from iron. It often takes 3-12 months to see hair loss improve after your iron stores are refilled. If you have to wait 6 months before you can even start, it might take well over a year to see it improve.
Realistic expectations are:
- Diet: 0 – 0.5 mg per day
- Supplements: 5 – 15 mg per day
- Infusions: up to 250 mg per infusion
If you need 750 mg of iron, diet would take (750 / 0.5) 1500 days (4.11 years) if everything worked perfectly. You could get a college degree by then! Or you could take supplements and maybe do it in under month.
What Action Steps Can You Take Today?
When it comes to iron, the first thing you should do is test. We often recommend screening your iron levels as a full panel, including:
- Ferritin
- CBC
- TIBC
- Transferrin
- Serum iron
The next thing you need to do is get a clear identification on your diagnosis. Are things normal? Do you have latent iron deficiency, iron deficiency anemia? Your test results will show.
Then, consider how great is your iron deficit and find out how long it will take to correct.
Iron deficiencies are common sources of symptoms. Sadly too many people try to treat low iron, don’t make progress and give up. They often assume their symptoms must be from some other cause because iron did not help.
Usually, the iron did not help because they never got corrected. Don’t give up on your health. Whatever the cause of your symptoms you can feel better if you take the right steps!
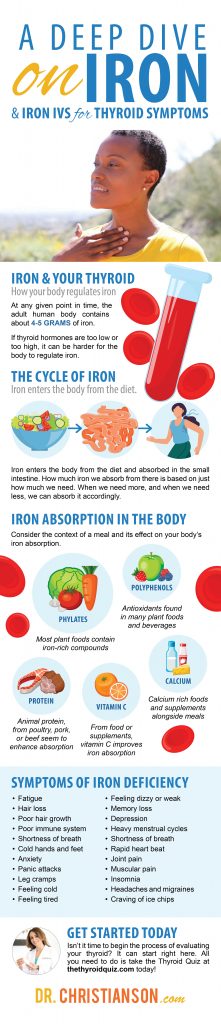
Start With Your Thyroid
Now that we know more about iron and its effect on common symptoms associated with thyroid disease, isn’t it time to begin the process of evaluating your thyroid?
It can start right here. All you need to do is take the Thyroid Quiz today (Click Here: Take The Thyroid Quiz). It can help uncover the truth about your thyroid, and what you can do to heal it starting today.
1 – https://www.ncbi.nlm.nih.gov/pubmed/17044765
2 – https://www.mdedge.com/endocrinology/article/104350/pituitary-thyroid-adrenal-disorders/iron-deficiency-may-explain
3 – https://www.ncbi.nlm.nih.gov/pubmed/4031012
4 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6166193/
5 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6166193/#ref36
6 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6166193/#ref38
7 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6166193/#ref39
8 – https://www.cdc.gov/ibd/data-statistics.htm
9 – https://www.ncbi.nlm.nih.gov/pubmed/1682595/
10 – https://medlineplus.gov/helicobacterpyloriinfections.html
11 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3925854/
12 – https://www.cdc.gov/ulcer/files/hpfacts.pdf
13 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2695884/
14 – https://www.ncbi.nlm.nih.gov/pubmed/15521972/
15 – https://www.ncbi.nlm.nih.gov/pubmed/15745105/
16 – https://www.ncbi.nlm.nih.gov/pubmed/15270751/
17 – https://www.ncbi.nlm.nih.gov/pubmed/32220343
P.S. Whenever you are ready, here is how I can help you now:
- Schedule a Thyroid Second Opinion with me, Dr. C, Click Here for Details
- Need help to choose supplements? Click ‘Help Me Decide Here'
- Get my top books Here
Dr. Alan Glen Christianson (Dr. C) is a Naturopathic Endocrinologist and the author of The NY Times bestselling Hormone Healing Cookbook, The Metabolism Reset Diet, and The Thyroid Reset Diet.
Dr. C’s gift for figuring out what works has helped hundreds of thousands reverse thyroid disease, heal their adrenals, and lose weight naturally. Learn more about the surprising story that started his quest.