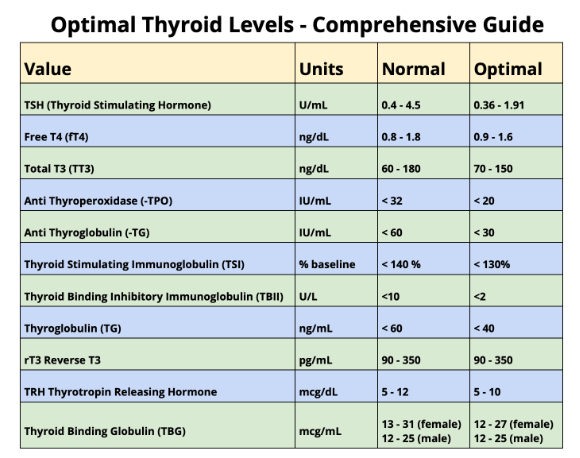
What Your Results Mean: Normal and Optimal Levels
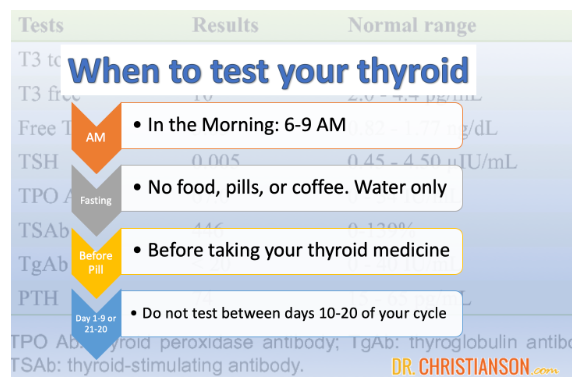
Single test?
When considering the results of your tests, the first thing I’d like you to know is that any one result can be a fluke.
There are many reasons why you can have a set of thyroid results that show up once but are different on a retest, even if the retest is only a few days later.
Never base a diagnosis or treatment on a single result. Over 30% of the time, someone with abnormal thyroid levels has perfectly normal results if they do nothing more than retest in a few weeks.
Get Help
Now that you have results, what do they mean? This blog will talk about each test and its normal and optimal ranges. Yet lab tests can only be intercepted in the context of your:
- Other lab tests
- Symptoms
- Health history
- Demographics
- Family history
- And more
You want guidance.
You can plug them into the Thyroid Lab Analyzer for automated help or consult with me in person for one-on-one guidance.
Normal vs. Optimal
I’ll talk about normal and optimal levels for each of these labs.
Normal levels are those printed on your lab report. They can vary from lab to lab, but these are generally average. Sometimes, average levels are not the best, especially for specific individuals.
Many health experts share lists of ‘optimal’ thyroid levels. I’m no exception, but I’d like you to take them all with a grain of salt.
- For most thyroid tests, it is never OK if the results are not normal
- You may be perfectly healthy with levels that are not optimal
- Optimal is not the same for all people
The valuable part of normal vs optimal is that some people needing thyroid medication feel better at some parts of the normal range than others. That’s OK.
Where optimal levels are misused is when:
- People are put on medication because their levels are not optimal
- People are given an overdose of medication, which pushes their TSH below range to make T3 ‘optimal’
With that said, let’s talk about the individual thyroid levels.
TSH
Normal
Most labs say the TSH is normal, between 0.4 and 4.5.
Optimal?
Some who need medication feel better when their TSH is low normal – as in 0.5 – 2.0. That’s OK.
Some people have hypothyroid symptoms when their TSH is above 2.0. That is real, but thyroid medications are not the answer.
Subclinical Hypothyroidism
If the TSH is elevated, but the T4 is still present, this is called subclinical hypothyroidism. It can cause hypothyroid symptoms, but medications rarely provide more benefit than risk. The Thyroid Reset Diet has been clinically proven to help the majority of people reverse suboptimal and subclinical hypothyroidism.
Overt Hypothyroidism
If the TSH is significantly elevated, as in 20-300, and the TT4 is well below range, the condition is usually overt hypothyroidism. This is true hypothyroidism. There is too little thyroid hormone. Medication is helpful and appropriate. Yet, some can still respond to dietary change without it.
If the TSH is below range, this is called hyperthyroidism. The most common reasons are too much thyroid medication or undiagnosed Graves’ disease.
There are risks for hyperthyroidism, such as:
- Brain damage
- Bone loss
- Heart disease
These risks are real even if T3 and T4 are not elevated.
Free Hormones (Free T4 and Total T3 Tests)
These both have a wide range of normal and many different units reported.
In general, things are acceptable if they are in range. Healthier populations tend to have them both mid-range or low normal.
Some health experts argue the opposite. They assume that since some people feel better with a low-normal TSH, they must have a high-normal T3. Given how much regulation T3 has, the one does not follow the other.
Human studies show that consistently high levels of T3 are a known risk for breast cancer and diabetes.
Furthermore, if one tries to use medication to raise T3 and/or T4 to high-normal – it pushes the TSH below range. This creates risks because TSH is needed to repair bones and blood vessels normally.
Thyroid Antibodies
Immune tests like thyroid antibodies are trickier. The same antibodies at the same level do not always act in the same way.
- Some people with Hashimoto’s never have measurable antibodies4
- Some with high antibodies never get Hashimoto’s
- Antibodies can fluctuate significantly from one test to the next
What can we say?
Anti-thyroglobulin is not as commonly high, but when it is, it is usually a cause of symptoms.
Anti-thyroid peroxidase is almost always a big deal in the 1000s.
Action steps for interpreting antibodies:
- Get help
- Don’t put too much weight on one reading
- If they are extremely high, consider nutraceuticals. Antibody Support has been clinically proven to help
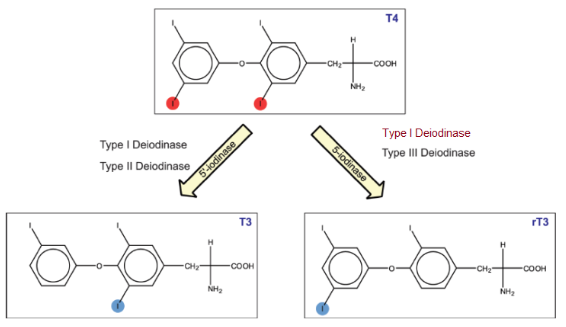
Reverse T3
I don’t routinely test rT3. Many perfectly healthy people have high or low levels of rT3. This is of no known significance.
Many people with thyroid problems have normal rT3.
If you have thyroid issues and elevated rT3, it can mean:
- Nothing – some labs have unusual ranges
- Overmedicated – your body will make more rT3 if your medication dose is too high
- Comorbidity – if your health is compromised in some way, your body may deactivate more thyroid hormone to slow your metabolism. The answer is not hacking rT3; it is fixing the comorbidity.