After thinking more thoroughly about the situation I realized something absolutely critical. While it was possible for treatment to make sense and produce initially positive results, it might not be moving someone towards better health in the long-term.
Does Your Body Want More Cortisol?
I thought about all the times and which doctors gave out cocaine or opium in the 1900’s, or Valium in the 60’s because of the benefits the patients had reported.
I realized that medications as powerful as hormones could be misused in the exact same ways.
How do you know that your body does not want more cortisol?
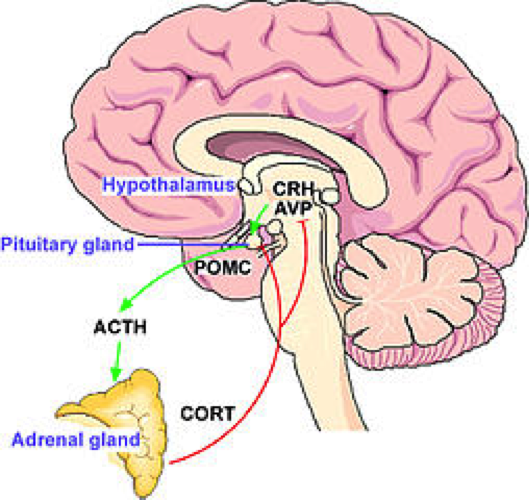
Thankfully, it is pretty simple – it is an ACTH blood test. Any doctor can order it and your doctor should order it to see why your cortisol levels might be low.
This test gives you an idea about the hormone that your brain makes to tell your adrenal glands to get to work – because your brain is under the assumption that not enough cortisol is being made.
Specifically, it comes from the pituitary gland after the hypothalamus releases a hormone called corticotropin. This stimulates the pituitary and causes all this to occur.